Start saving with the
RYTARY Co-Pay Savings Card.

If you have commercial insurance, you may be eligible to:
Pay as little as $25
for your first RYTARY prescription*
Pay as little as $0
if you’re written a second or third prescription of RYTARY within that same 30-day period†
Real people. Real RYTARY stories.
Get information to help you on your journey.
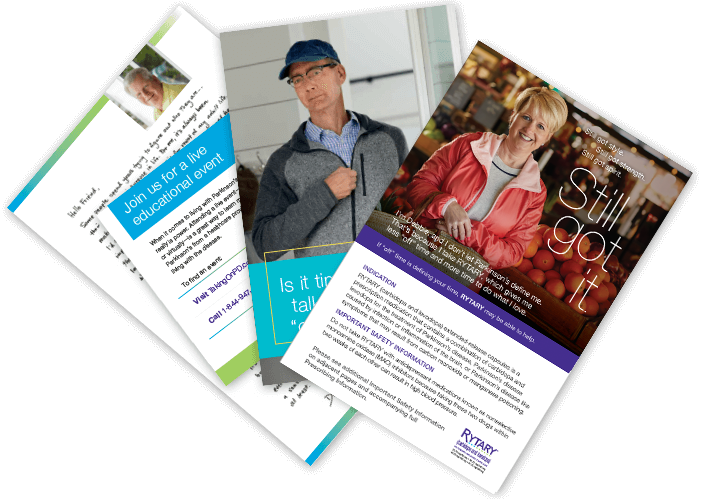
From considering RYTARY to starting treatment, people with Parkinson’s and their care partners can sign up for free resources, ongoing communications, and more.
Get RYTARY—a Parkinson’s
medication
that can help
the real you shine through.
- After switching to RYTARY, people had significantly less “off” time than they did when taking IR
CD/LD
— Percentage of “off” time at study start and study end: 36.9% and 23.8% with RYTARY vs 36.0% and 29.8% with IR CD/LD‡
- After switching to RYTARY, people had significantly more “on” time without troublesome
dyskinesia
than they did when taking IR CD/LD
— 1.8 hours with RYTARY vs 0.8 hours with IR CD/LD¶
- After switching to RYTARY, people also experienced a significant improvement in motor functions, which can help when performing daily activities
- A different analysis of the same study found that optimized RYTARY provided more hours per dose
of
“on” time compared to optimized IR CD/LD
— Hours of “on” time per dose at baseline and study end: 2.17 and 3.55 with RYTARY vs 2.24 and 2.38 with IR CD/LD
In a clinical study, the most common side effects occurring in at least 5% of people treated with RYTARY and at a higher rate than IR CD/LD were nausea and headache.
‡Study end=Week 22 or early termination; P<0.0001 vs IR CD/LD.§These were secondary measures of the study.
¶P=0.0002 vs IR CD/LD.
**This was a post hoc analysis of the study; P<0.0001 vs IR CD/LD.
You are not your disease.
You are a unique individual who happens to have Parkinson’s.
So let your story be heard.
Be your own health advocate.Denise, on RYTARY since 2016
†This card is not valid for prescriptions submitted for reimbursement to Medicare, Medicaid, other federal or state programs (including any state pharmaceutical assistance programs), or private indemnity or HMO insurance plans that reimburse you for the entire cost of your prescription drugs. This card is good for use only with a RYTARY prescription at the time the prescription is filled by the pharmacist and dispensed to the patient. Offer good only in the USA at participating retail pharmacies. Void if prohibited by law, taxed, or restricted. The selling, purchasing, trading, or counterfeiting of this card is prohibited by law. This card is good for up to 3 prescription fills per month.